Search
- Page Path
- HOME > Search
- Clinical Study
- Insulin Secretion and Insulin Resistance Trajectories over 1 Year after Kidney Transplantation: A Multicenter Prospective Cohort Study
- Jun Bae Bang, Chang-Kwon Oh, Yu Seun Kim, Sung Hoon Kim, Hee Chul Yu, Chan-Duck Kim, Man Ki Ju, Byung Jun So, Sang Ho Lee, Sang Youb Han, Cheol Woong Jung, Joong Kyung Kim, Su Hyung Lee, Ja Young Jeon
- Endocrinol Metab. 2020;35(4):820-829. Published online November 18, 2020
- DOI: https://doi.org/10.3803/EnM.2020.743
- 4,964 View
- 119 Download
- 5 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
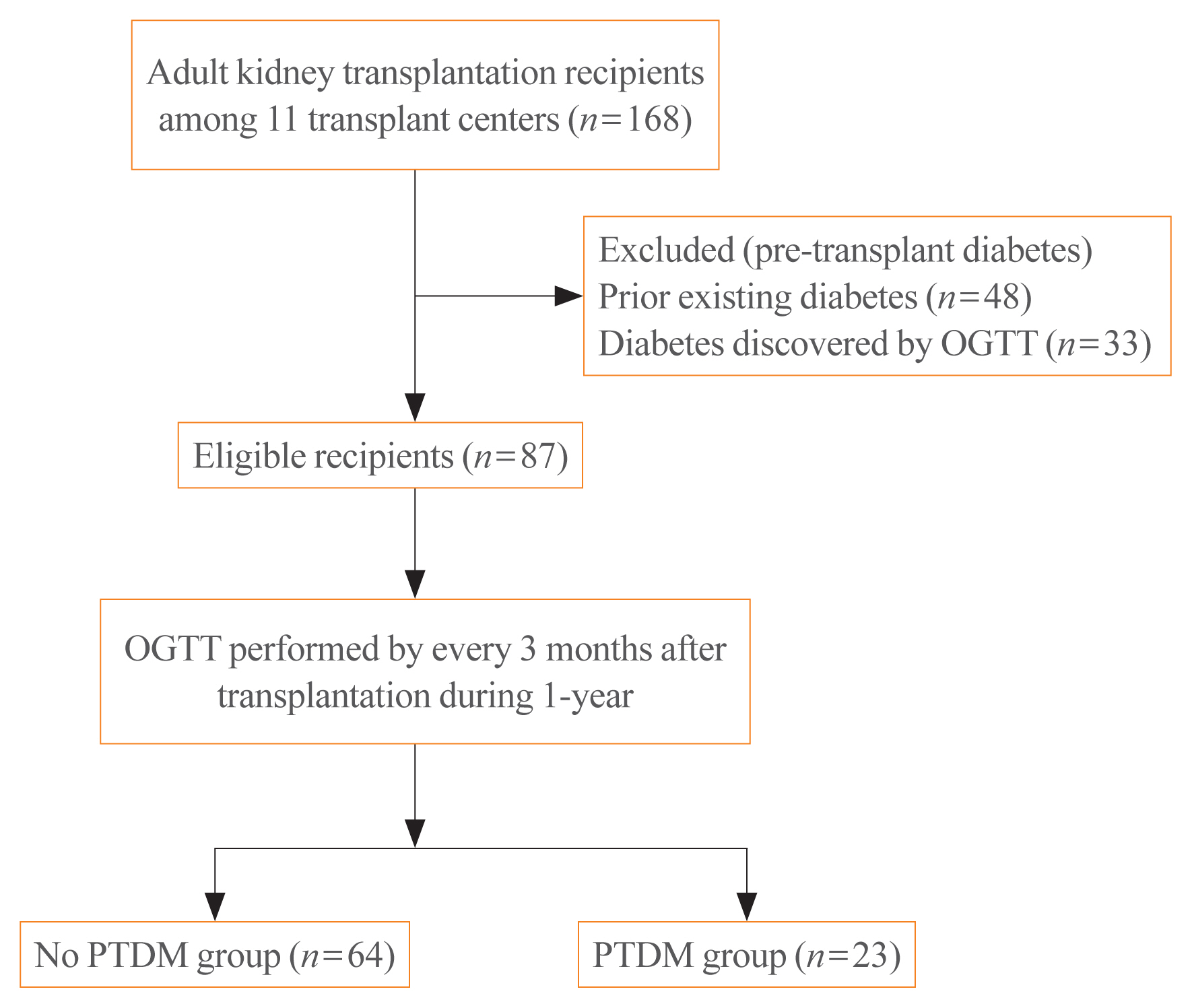
We investigated the changing patterns of insulin secretion and resistance and risk factors contributing to the development of post-transplant diabetes mellitus (PTDM) in kidney recipients under tacrolimus-based immunosuppression regimen during 1 year after transplantation.
Methods
This was a multicenter prospective cohort study. Of the 168 subjects enrolled in this study, we analyzed a total 87 kidney transplant recipients without diabetes which was assessed by oral glucose tolerance test before transplantation. We evaluated the incidence of PTDM and followed up the index of insulin secretion (insulinogenic index [IGI]) and resistance (homeostatic model assessment for insulin resistance [HOMA-IR]) at 3, 6, 9 months, and 1 year after transplantation by oral glucose tolerance test and diabetes treatment. We also assessed the risk factors for incident PTDM.
Results
PTDM developed in 23 of 87 subjects (26.4%) during 1 year after transplantation. More than half of total PTDM (56.5%) occurred in the first 3 months after transplantation. During 1 year after transplantation, insulin resistance (HOMA-IR) was increased in both PTDM and no PTDM group. In no PTDM group, the increase in insulin secretory function to overcome insulin resistance was also observed. However, PTDM group showed no increase in insulin secretion function (IGI). Old age, status of prediabetes and episode of acute rejection were significantly associated with the development of PTDM.
Conclusion
In tacrolimus-based immunosuppressive drugs regimen, impaired insulin secretory function for reduced insulin sensitivity contributed to the development of PTDM than insulin resistance during 1 year after transplantation. -
Citations
Citations to this article as recorded by- Prevalence of new-onset diabetes mellitus after kidney transplantation: a systematic review and meta-analysis
Qiufeng Du, Tao Li, Xiaodong Yi, Shuang Song, Jing Kang, Yunlan Jiang
Acta Diabetologica.2024;[Epub] CrossRef - Distúrbio do eixo hipotálamo-hipófise-gonadal e sua associação com resistência à insulina em receptores de transplante renal
Lourdes Balcázar-Hernández, Victoria Mendoza-Zubieta, Baldomero González-Virla, Brenda González-García, Mariana Osorio-Olvera, Jesús Ubaldo Peñaloza-Juarez, Irene Irisson-Mora, Martha Cruz-López, Raúl Rodríguez-Gómez, Ramón Espinoza-Pérez, Guadalupe Varga
Brazilian Journal of Nephrology.2023; 45(1): 77. CrossRef - Hypothalamic-pituitary-gonadal axis disturbance and its association with insulin resistance in kidney transplant recipients
Lourdes Balcázar-Hernández, Victoria Mendoza-Zubieta, Baldomero González-Virla, Brenda González-García, Mariana Osorio-Olvera, Jesús Ubaldo Peñaloza-Juarez, Irene Irisson-Mora, Martha Cruz-López, Raúl Rodríguez-Gómez, Ramón Espinoza-Pérez, Guadalupe Varga
Brazilian Journal of Nephrology.2023; 45(1): 77. CrossRef - Postoperative fasting plasma glucose and family history diabetes mellitus can predict post-transplantation diabetes mellitus in kidney transplant recipients
Le Wang, Jin Huang, Yajuan Li, Kewei Shi, Sai Gao, Wangcheng Zhao, Shanshan Zhang, Chenguang Ding, Wei Gao
Endocrine.2023; 81(1): 58. CrossRef - Changes in glucose metabolism among recipients with diabetes 1 year after kidney transplant: a multicenter 1-year prospective study
Jun Bae Bang, Chang-Kwon Oh, Yu Seun Kim, Sung Hoon Kim, Hee Chul Yu, Chan-Duck Kim, Man Ki Ju, Byung Jun So, Sang Ho Lee, Sang Youb Han, Cheol Woong Jung, Joong Kyung Kim, Hyung Joon Ahn, Su Hyung Lee, Ja Young Jeon
Frontiers in Endocrinology.2023;[Epub] CrossRef - Pretransplant evaluation and the risk of glucose metabolic alterations after renal transplantation: a prospective study
Arminda Fariña-Hernández, Domingo Marrero-Miranda, Estefania Perez-Carreño, Antonia De Vera-Gonzalez, Alejandra González, Cristian Acosta-Sorensen, Ana Elena Rodríguez-Rodríguez, Tatiana Collantes, Marta del Pino García, Ana Isabel Rodríguez-Muñoz, Carla
Nephrology Dialysis Transplantation.2022;[Epub] CrossRef
- Prevalence of new-onset diabetes mellitus after kidney transplantation: a systematic review and meta-analysis

- Endocrine Research
- The Role of Nuclear Factor-E2-Related Factor 1 in the Oxidative Stress Response in MC3T3-E1 Osteoblastic Cells
- So Young Park, Sung Hoon Kim, Hyun Koo Yoon, Chang Hoon Yim, Sung-Kil Lim
- Endocrinol Metab. 2016;31(2):336-342. Published online April 25, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.2.336
- 3,973 View
- 61 Download
- 10 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Reactive oxygen species (ROS) and antioxidants are associated with maintenance of cellular function and metabolism. Nuclear factor-E2-related factor 1 (NFE2L1, Nrf1) is known to regulate the expression of a number of genes involved in oxidative stress and inflammation. The purpose of this study was to examine the effects of NFE2L1 on the response to oxidative stress in osteoblastic MC3T3-E1 cells.
Methods The murine calvaria-derived MC3T3-E1 cell line was exposed to lipopolysaccharide (LPS) for oxidative stress induction. NFE2L1 effects were evaluated using small interfering RNA (siRNA) for
NFE2L1 mRNA. ROS generation and the levels of known antioxidant enzyme genes were assayed.Results NFE2L1 expression was significantly increased 2.4-fold compared to the control group at 10 µg/mL LPS in MC3T3-E1 cells (P <0.05). LPS increased formation of intracellular ROS in MC3T3-E1 cells.NFE2L1 knockdown led to an additional increase of ROS (20%) in the group transfected withNFE2L1 siRNA compared with the control group under LPS stimulation (P <0.05). RNA interference ofNFE2L1 suppressed the expression of antioxidant genes including metallothionein 2, glutamatecysteine ligase catalytic subunit, and glutathione peroxidase 1 in LPS-treated MC3T3-E1 cells.Conclusion Our results suggest that NFE2L1 may have a distinct role in the regulation of antioxidant enzymes under inflammation-induced oxidative stress in MC3T3-E1 osteoblastic cells.
-
Citations
Citations to this article as recorded by- SDH5 down-regulation mitigates the damage of osteoporosis via inhibiting the MyD88/NF-κB signaling pathway
Hongzi Wu, Dehua Zhang, Haijun Xia, Yongqi Li, Feng Mao, Yi Liao
Immunopharmacology and Immunotoxicology.2023; 45(3): 317. CrossRef - N-acetyl Cysteine Inhibits Cell Proliferation and Differentiation of LPSInduced MC3T3-E1 Cells Via Regulating Inflammatory Cytokines
Wangyang Li, Hui Zhang, Junchi Chen, Yujie Tan, Ailing Li, Ling Guo
Current Pharmaceutical Biotechnology.2023; 24(3): 450. CrossRef - Unravelling the role of NFE2L1 in stress responses and related diseases
Xingzhu Liu, Chang Xu, Wanglong Xiao, Nianlong Yan
Redox Biology.2023; 65: 102819. CrossRef - Nfe2l1 deficiency mitigates streptozotocin-induced pancreatic β-cell destruction and development of diabetes in male mice
Simeng Bao, Hongzhi Zheng, Chengjie Chen, Yuhang Zhang, Lina Bao, Bei Yang, Yongyong Hou, Yanyan Chen, Qiang Zhang, Jingbo Pi, Jingqi Fu
Food and Chemical Toxicology.2021; 158: 112633. CrossRef - Long isoforms of NRF1 negatively regulate adipogenesis via suppression of PPARγ expression
Peng Xue, Yongyong Hou, Zhuo Zuo, Zhendi Wang, Suping Ren, Jian Dong, Jingqi Fu, Huihui Wang, Melvin E. Andersen, Qiang Zhang, Yuanyuan Xu, Jingbo Pi
Redox Biology.2020; 30: 101414. CrossRef - Protracted rosiglitazone treatment exacerbates inflammation in white adipose tissues of adipocyte-specific Nfe2l1 knockout mice
Suping Ren, Yongyong Hou, Zhuo Zuo, Zhiyuan Liu, Huihui Wang, Yuanyuan Xu, Masayuki Yamamoto, Qiang Zhang, Jingqi Fu, Jingbo Pi
Food and Chemical Toxicology.2020; 146: 111836. CrossRef - Nrf1 is paved as a new strategic avenue to prevent and treat cancer, neurodegenerative and other diseases
Jianxin Yuan, Shuwei Zhang, Yiguo Zhang
Toxicology and Applied Pharmacology.2018; 360: 273. CrossRef - Silencing of long isoforms of nuclear factor erythroid 2 like 1 primes macrophages towards M1 polarization
Huihui Wang, Jiayu Zhu, Zhiyuan Liu, Hang Lv, Peng Lv, Feng Chen, Jingqi Fu, Yongyong Hou, Rui Zhao, Yuanyuan Xu, Qiang Zhang, Jingbo Pi
Free Radical Biology and Medicine.2018; 117: 37. CrossRef - Costunolide increases osteoblast differentiation via ATF4-dependent HO-1 expression in C3H10T1/2 cells
Wan-Jin Jeon, Kyeong-Min Kim, Eun-Jung Kim, Won-Gu Jang
Life Sciences.2017; 178: 94. CrossRef
- SDH5 down-regulation mitigates the damage of osteoporosis via inhibiting the MyD88/NF-κB signaling pathway

- Thyroid
- Thyroid Dysfunction Associated with Administration of the Long-Acting Gonadotropin-Releasing Hormone Agonist
- Eun Jin Han, Ha Do Song, Ji Hoon Yang, So Young Park, Sung Hoon Kim, Hyun Koo Yoon, Chang Hoon Yim
- Endocrinol Metab. 2013;28(3):221-225. Published online September 13, 2013
- DOI: https://doi.org/10.3803/EnM.2013.28.3.221
- 4,530 View
- 47 Download
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Gonadotropin-releasing hormone (GnRH) agonist has been used in the treatment of a wide variety of sex-hormone-related diseases, as the administration of GnRH agonist can alter the secretion of gonadotropin and sex hormones. Recently, we found that the long-acting GnRH agonist aggravated hyperthyroidism and induced painless thyroiditis. This is the first report to demonstrate the association of thyroid dysfunction with GnRH agonist injection in Korea. Here, we report three cases and emphasize the clinical importance of this aggravating factor in autoimmune thyroid disease.
-
Citations
Citations to this article as recorded by- Thyroid Dysfunction after Gonadotropin-Releasing Hormone Agonist Administration in Women with Thyroid Autoimmunity
Loris Marin, Guido Ambrosini, Marco Noventa, Flavia Filippi, Eugenio Ragazzi, Francesco Dessole, Giampiero Capobianco, Alessandra Andrisani, Alexander Schreiber
International Journal of Endocrinology.2022; 2022: 1. CrossRef - Effects of controlled ovarian stimulation on thyroid function during pregnancy
Lingfei Li, Ling Li, Ping Li
Biology of Reproduction.2022; 107(6): 1376. CrossRef - Is gonadotropin-releasing hormone agonist usage really leading to thyroid dysfunction?
Nafiye Yilmaz, Necati Hancerliogullari, Mustafa Kara, Yaprak Engin-Ustun
Interventional Medicine and Applied Science.2020; 11(3): 136. CrossRef - FANCA Polymorphism Is Associated with the Rate of Proliferation in Uterine Leiomyoma in Korea
Eunyoung Ha, Seungmee Lee, So Min Lee, Jeeyeon Jung, Hyewon Chung, Eunsom Choi, Sun Young Kwon, Min Ho Cha, So-Jin Shin
Journal of Personalized Medicine.2020; 10(4): 228. CrossRef - Effects of controlled ovarian stimulation on thyroid stimulating hormone in infertile women
Yuan-Jie Du, Xin Xin, Na Cui, Lei Jiang, Ai-Min Yang, Gui-Min Hao, Bu-Lang Gao
European Journal of Obstetrics & Gynecology and Reproductive Biology.2019; 234: 207. CrossRef - Myxedema Coma Following the Administration of Gonadotropin-releasing Hormone Agonist Complicated by Acute Pancreatitis
Naoki Gocho, Ema Aoki, Chiho Okada, Takeshi Hirashima
Internal Medicine.2018; 57(21): 3117. CrossRef - The impact of thyroid autoimmunity on IVF/ICSI outcome: a systematic review and meta-analysis
Andrea Busnelli, Alessio Paffoni, Luigi Fedele, Edgardo Somigliana
Human Reproduction Update.2016; 22(6): 775. CrossRef - The Potential Role of GnRH Agonists and Antagonists in Inducing Thyroid Physiopathological Changes During IVF
Salvatore Gizzo, Marco Noventa, Michela Quaranta, Amerigo Vitagliano, Federica Esposito, Alessandra Andrisani, Roberta Venturella, Carlo Alviggi, Mario Plebani, Michele Gangemi, Giovanni Battista Nardelli, Donato D’Antona
Reproductive Sciences.2016; 23(4): 515. CrossRef - Brief Review of Articles in 'Endocrinology and Metabolism' in 2013
Won-Young Lee
Endocrinology and Metabolism.2014; 29(3): 251. CrossRef
- Thyroid Dysfunction after Gonadotropin-Releasing Hormone Agonist Administration in Women with Thyroid Autoimmunity

- A Case of Hypothyroidism in Remission during Pregnancy.
- Ha Do Song, Eun Jin Han, Sung Ja Lee, Ji Hoon Yang, So Young Park, Sung Hoon Kim, Ki Ok Han, Hyun Koo Yoon, Chang Hoon Yim
- Endocrinol Metab. 2012;27(4):295-298. Published online December 20, 2012
- DOI: https://doi.org/10.3803/EnM.2012.27.4.295
- 2,175 View
- 38 Download
-
 Abstract
Abstract
 PDF
PDF - Hypothyroidism should be treated in pregnancy, because it has been associated with an increased risk of adverse pregnancy complications, as well as detrimental effects upon fetal neurocognitive development. The goal of L-thyroxine (LT4) treatment is to normalize maternal serum TSH values within the trimester-specific pregnancy reference range. 50% to 85% of hypothyroid women being treated with exogenous LT4 need to increase the dose during pregnancy. In this study, we report a case of a 29-year-old woman with hypothyroidism who had been in remission and discontinued LT4 treatment during her pregnancy. Three months after delivery she had a relapse of hypothyroidism and was retreated with LT4. Many factors can influence the gestational requirement for LT4, therefore maternal serum TSH should be monitored and the LT4 dose should be adjusted in pregnant patients with treated hypothyroidism.

- The Change of Insulin Sensitivity and Insulin Secretion According to Glucose Metabolism Status in Patients with Cushing's Syndrome.
- In Kyung Jeong, Sung Hoon Kim, Jae Hoon Chung, Yong Ki Min, Myung Shik Lee, Moon Kyu Lee, Hyung Joon Yoo, Kyu Jeong Ahn, Jung Hynun Noh, Dong Jun Kim, Kwang Won Kim
- J Korean Endocr Soc. 2003;18(4):392-403. Published online August 1, 2003
- 1,075 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Glucocorticoid plays an important role in the control of carbohydrate metabolism. Patients with Cushing's syndrome have been reported to have an increased incidence of carbohydrate intolerance due to peripheral insulin resistance and hyperinsulinemia, although the exact incidence and nature of this disorder have remained unclear. Few results have been published about insulin resistance and insulin secretion according to the level of glucose concentration, or about the reversibility of such defects in patients with Cushing's syndrome. METHODS: To assess the effect of glucocorticoid on the insulin sensitivity and insulin secretion in Cushing's syndrome, 15 patients with Cushing's syndrome were classified into 3 groups (normal glucose tolerance: NGT, impaired glucose tolerance: IGT, diabetes: DM) according to the degree of glucose tolerance based on the oral glucose tolerance test (OGTT). Insulin modified, frequentlysampled, intravenous glucose tolerance test (FSIGT) was performed before and after curative surgery on these patients and on 15 healthy control subjects. Data were evaluated by non-parametric statistical analysis. RESULTS: 1) Among the 15 patients with Cushing's syndrome, 3 (20%) were NGT, 4 (27%) IGT, and 8 (53%) DM, based on OGTT. Twenty-four hour urinary free cortisol (UFC) was significantly higher in the DM group. 2) Insulin sensitivity index (SI) of Cushing's syndrome was significantly lower than that of the control group (P=0.0024), but was not significantly different among the three Cushing's syndrome groups of NGT, IGT and DM. 3) Glucose mediated glucose disposal (SG) (Ed- confirm this abbreviation; it does not seem to match the definition) of Cushing's syndrome was not significantly different from that of the control group. 4) Insulin secretion (AIRg) of Cushing's syndrome tended to be high, but it was not significantly different from that of control. However, according to the level of glucose concentration there was significant difference in AlRg among the three Cushing's syndrome groups (P=0.0031); AIRg of DM was significantly lower than that of NGT. 5) After surgical treatment, parameters of insulin sensitivity and insulin secretion were normalized in 6 cured patients; 1 with NGT, 1 with IGT, and 4 with DM, preoperatively. Median SI of all 6 patients was significantly improved up to the normal range postoperatively (P=0.0022). Median AIRg of these 6 patients was balanced around that of normal control postoperatively (P=0.0286). CONCLUSION: Eighty percent of patients with Cushing's syndrome had abnormality of carbohydrate metabolism. Insulin sensitivity was significantly decreased in Cushing's syndrome. Insulin secretion was significantly higher only in the NGT and IGT groups of Cushing's syndrome. As the hypercortisolemia is exacerbated, insulin secretion is significantly decreased and causes DM, suggesting that glucocorticoid has a direct or indirect toxic effect on the pancreatic beta cell.

- A Case of Islets Cell Hyperplasia Diagnosed by Selective Arterial Calcium Stimulation Test.
- Jin Hoon Youn, Kyu Jeung Ahn, Yeong Shil Joo, Byoung Joon Kim, Sung Hoon Kim, Kye Hyoung Kwon, Myung Ah Jung, Jin Soo Yang, In Su Jung, Chung Hyeon Kim, Sung Bum Cho, Tae Seok Lee, Eun Kyung Kim
- J Korean Endocr Soc. 2001;16(4-5):514-519. Published online October 1, 2001
- 1,028 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - We report a 40-year-old female patient with clinical findings suggestive of insulinoma. Although imaging studies did not reveal any tumors in the pancreas, a selective arterial calcium stimulation test(SACI), procedurally simpler and more effective than transhepatic pancreatic venous sampling, was performed. And then near total pancreatectomy was carried out because the possibility of small insulinoma could not be completely excluded. Grossly, the surgically removed pancreas did not reveal any tumors. However, the pancreas exhibited islets cell hyperplasia. To our knowledge, this is the first reported authentic case in a Korean adult of islet-cell hyperplasia diagnosed by selective arterial calcium stimulation test.

- A Case of Osteomalacia with Long Term Carbamazepine Therapy.
- Hee Soo Kim, Dong Sun Kim, Nak Won Choi, Sang Hyun Baik, Sung Hoon Kim, Chang Beom Lee, Yong Soo Park, Woong Hwan Choi, You Hern Ahn, Tae Hwa Kim
- J Korean Endocr Soc. 2000;15(2):286-290. Published online January 1, 2001
- 1,240 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - Anticonvusant therapy with any of several agents, especially phenytoin, phenobarbital, and primidone causes disturbances in bone mineral metabolism. Anticonvulsants stimulate the hepatic microsomal mixed-oxidase enzymes and hence increase the rate of clearance of vitamin D and its metabolism. The severity of clinical manifestations in any given individual appears to be a function of the combined effects of variety of factors including drug type and total drug dose, dietary vitamin D intake, sunlight exposure, and physical activity level. We report a case of osteomalacia associated with long term carbamazepine therapy in a 21-year-old male with less exposure to sunlight.

- Routine Measurement of Serum Calcitonin Concentration is Useful in Early Detection of Medullary Thyroid Carcinoma Among Patients with Nodular Thyroid Disease.
- Jong Ryeal Hahm, Jae Hoon Chung, Eun Young Oh, In Kyung Chung, Tae Young Yang, Dong Jun Kim, Byung Ju Kim, Sung Hoon Kim, Yong Ki Min, Myung Shik Lee, Moon Kyu Lee, Kwang Won Kim
- J Korean Endocr Soc. 2000;15(1):70-84. Published online January 1, 2001
- 1,179 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Serum calcitonin is a sensitive and specific marker for diagnosis of medullary thyroid carcinoma (MTC) and its determination leads to accurate preoperative diagnosis and gives chances of definite cure. However, since many non-MTC diseases are also associated with calcitonin elevation, its significance in patients with mild or moderately elevated basal serum calcitonin levels is not clear. Furthermore, the normal value of calcitonin using immunoradiometric assay (IRMA) kit has not so far been definitely ascertained. This study is aimed at assessing the clinical significance of routine measurement of serum basal calcitonin concentration in nodular thyroid disease patients and evaluating the pentagastrin stimulation test in case of mild or moderate elevation of basal calcitonin level. We also measured serum calcitonin value in 408 normal individuals. METHODS: The basal serum calcitonin concentrations using a commercial IRMA kit (Medgenix CT-U.S.-IRMA) were measured in 818 patients with nodular thyroid disease (average age 45 years with a range from 13 to 82 years; 125 males and 693 females) who visited thyroid clinics in Samsung Medical Center between June 1997 and December 1998. Serum concentrations of T3, T4, TSH and thyroid autoantibodies were measured and ultrasonography of thyroid and thyroid scan using 131I or 99mTc-pertechnetate were performed in all patients. We also studied 408 healthy subjects without any thyroid disease (average age 48 years with a range from 20 to 86 years; 224 females). RESULTS: The calcitonin value in normal subjects was found to range from 0 to 13 pg/mL, and it was shown that men had higher calcitonin level than women (p< 0.05). The rate of serum calcitonin elevation (> 10pg/mL) in nodular thyroid disease was 1.71% (14/818), and the incidence of MTC was 0.73% (6/818) in this study. MTC was found in all patients with basal serum calcitonin levels more than 100 pg/mL. Pentagastrin stimulation test was also required to diagnose MTC in patients with basal serum calcitonin levels between 30 and 100pg/mL. The calcitonin concentration stimulated by pentagastrin increased more than 400pg/mL or more than 3.8 times of basal concentration. It was possible to diagnose MTC with fine needle aspiration and cytology in only one case out of six patients with MTC. CONCLUSION: Fine needle aspiration and cytology in diagnosing MTC was not sensitive and not devoid of false positive results. We confirmed that serum calcitonin measurement was very useful means for the preoperative diagnosis of unsuspected MTC. Pentagastrin stimulation test may be a reliable means of evaluation in nodular thyroid disease patients with mild or moderate elevation of basal calcitonin level. We recommend routine measurement of serum calcitonin concentration in patients with nodular thyroid disease.

- Cholesterol Lowering Effect of Cerivastatin in Korean Patients with Primary Hypercholesterolemia.
- Sung Hoon Kim, Dong Jun Kim, Jong Rhulk Hahm, Byung Joon Kim, Jae Hoon Chung, Yong Ki Min, Myung Shik Lee, Moon Kyu Lee, Kwang Won Kim
- J Korean Endocr Soc. 1999;14(4):729-738. Published online January 1, 2001
- 1,251 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Cerivastatin is a kind of statin, a synthetic HMG-CoA reductase inhibitor with high liver selectivity which lowers plasma cholesterol level by inhibiting endogenous cholesterol synthesis. This study evaluates the efficacy, safety, and tolerability of cerivastatin 0.1 mg and 0.3 mg in Korean patients with primary hypercholesterolemia. METHODS: A parallel group, randomized, placebo-controlled, double-blind study was conducted at Samsung Medical Center. The patients with primary hypercholesterolemia were placed on an American Heart Association Step 1 diet for whole study period. Single-blind placebo was administered for the final 4 weeks of period A, before randomization. Thirty two patients with low-density lipoprotein cholesterol (LDL-C) >160 mg/dL (if patients with a definite personal history of coronary heart disease (CHD) or with two or more cardiovascular risk factors, LDL-C >130 mg/dL) were randomized to 6 weeks treatment with one of the following regimens: cerivastatin 0.1 mg (n=11) or cerivastatin 0.3 mg (n=10) or placebo once daily at bedtime (n=11). RESULTS: Cerivastatin 0.1 mg and 0.3 mg treatment groups produced statistically significant (p<.05) changes at 6 weeks after treatment, compared to baseline and placebo in LDL-C (cerivastatin 0.1 mg 16.3%; cerivastatin 0.3 mg 35.2%; placebo 1.5%) and total cholesterol (cerivastatin 0.1 mg 10.3%; cerivastatin 0.3 mg 26.2%; placebo 1.3%). Cerivastatin 0.1 mg and 0.3 mg treatments were well tolerated and resulted in no significant increase in biochemical or clinical side effects compared to placebo. CONCLUSION: Cerivastatin at doses of 0.1 mg and 0.3 mg/day is a safe, well-tolerated, and highly effective HMG-CoA reductase inhibitor for the treatment of primary hypercholesterolemia.

- A Case of Diabetes Mellitus Caused by Calcitonin and Somatostatin Secreting Pancreatic Islet Tumor.
- Jae Hoon Chung, Kwang Won Kim, Byoung Joon Kim, Sung Hoon Kim, Kyung Ah Kim, Myung Sik Lee, Moon Gyu Lee, Yong Ki Min, Jong Ryol Ham, Dong Joon Kim, Hoe Jung Lee, Young Ryoon Oh
- J Korean Endocr Soc. 1999;14(2):425-431. Published online January 1, 2001
- 1,045 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - A case of 39-year-old diabetic patient with a calcitonin and somatostatin secreting pancreatic islet tumor is presented. He had suffered from chronic diarrhea and dyspepsia for 10 years and was diagnosed with diabetes 2 years ago. Abdominal CT revealed a huge abdominal mass which was considered as a neuroendocrine tumor after US-guided needle biopsy. A distal pancreatectomy and splenectomy were performed. Histologically, tumor cells, amanged in solid sheets, showed small nuclei without significant atypia and granular eosinophilic cytoplasm. Tumor cells showed strong immunoreacitivity for calcitonin and somatostatin. The serum clacitonin was markedly elevated (268.7 pmol/L, normal range; 0.9-7.6 pmol/L). After resection of the tumor, diarrhea and dyspepsia diappeared, and oral glucose tolerance test showed normal glucose tolerance with normalization of calcitonin.

- Prevalence of Thyrotoxicosis and Hypothyroidism in the Subjects for Health Check-Up.
- Jae Hoon Chung, Byoung Joon Kim, Yun Ho Choi, Myung Hee Shin, Sung Hoon Kim, Yong Ki Min, Myung Sik Lee, Moon Gyu Lee, Kwang Won Kim
- J Korean Endocr Soc. 1999;14(2):301-313. Published online January 1, 2001
- 1,100 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The prevalence of ovat hyperthyroidism ar hypothyroidism has been estimated up to 5% in the general populatian. Subclinical hyperthyroidism and subclinical hypothyroidism have pevalences of approximately 1% and 6%, ectively. The prevalence of hypothyroidism may be associated with excessive intake of iodine in iodine sufficient areas. Therefore, we assumed the prevalence of thyroid dysfunction in Karea might be different from those af Western cauntries. However, thete have been no surveys to examine the prevalence of thyroid dysfunction in Karea. We performed the study to investigate the prevalence of thyrotoxicosis and hypothyroidism in Korean adults. METHODS: This study was performed in 15019 subjects (8275 men, 6744 women; between 17 and 87 years of age) visited in health promotion center of Samsung Medical Center for 12 months in 1996. Serum T3, T4, and TSH concentrations were measured with RIA or IRMA using commercial kits. History of thyroid dysfunction and current medication were obtained from medical records. The criteria for thyrotoxicosis were TSH level below than 0.30 mU/L and increased T3 or T4 levels (T3 > 3.1 nmol/L or T4 > 152 nmol/L). Patients who had TSH level above than 5.0 mU/L and T4 level below than 77 nmol/L met the criteria for hypothyroidism. RESULTS: The prevalence of thyrotoxicosis was 5.5/1000 population (men 3.6/1000, women 7.7/1000) with peak prevalence in fifth decade. The prevalence of previously undiagnosed thyrotoxicosis was 4.0/1000 (men 2.9/1000, women 5.3/1000). The prevalence of hypothyroidism was 2.8/1000 population (men 1.1/1000, women 4.9/1000) with peak prevalence in seventh decade. The prevalence of previously undiagnosed hypothyroidism was 1.6/1000 (men 0.6/1000, women 2.S/1000). The prevalence of subclinical thyrotoxicosis was 12.4/1000 population (men 11.8/1000, women 13.0/1000). The prevalence of subclinical hypothyroidism was 18.2/1000 population (men 11.2/1000, women 26.7/1000) which frequency was increased with age. CONCLUSION: Although the prevalence of thyrotoxicosis and hypothyroidism was not significantly different from those of other countries, it was lower than expected and female preponderance is not significant. The prevalence of subclinical thyrotoxicosis and subclinical hypothyroidism was lower than those of other countries. The prevalence of subclinical hypothyroidism was higher in women and old ages. (J Kor Soc Endecrinol 14:301~313, 1999)

- ret/PTC-1, -2, and -3 Incogene Rearrangements of Papillary Thyroid Carcinomas in Korea and Its Relevance to Clinical Aggressiveness.
- Jong Ryeal Hanhm, Jae Hoon Chung, Byung Joon Kim, Kyoung Ah Kim, Sung Hoon Kim, Dong Jun Kim, Yong Ki Min, Myung Shik Lee, Moon Kyu Lee, Kwang Won Kim, Seok Jin Nam, Jung Hyun Yang, Howe Jung Ree
- J Korean Endocr Soc. 1999;14(1):53-62. Published online January 1, 2001
- 1,074 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The prevalence of ret/PTC rearrangement in papillary thyroid carcinomas has been found to have wide variance in different populations. Recent studies, however, have been reporting no significant geographical difference between Asian and Western countries. In addition, there are some arguments about the correlation of ret/PTC expression with clinical aggressiveness. We have performed this study in order to examine the prevalence of ret/PTC-1, -2 and -3 rearrangements in korean papillary throid carcinomas and to ascertain its clinical relevance. METHODS: Fourteen thyroid tumors histologically confirmed to be papillary carcinomas were included in this study. To find rearrangements, we adopted RT-PCR and automated direct sequencing. Initial and follow-up clinical data were obtained form the patients medical records. The plasmid containing ret/PTC-2, and 3 was kindly provided by Dr. Ahn (Ulsan University, Seoul Choonang Hospital). RESULTS: We identified one tumors containing ret/PTC-1(1/14, 7.1%), and two containing ret/PTC-2 (2/14, 14.2%), and could not find ret/PTC-3 rearrangement in other patients (0/11). There was no significant correlation of ret/PTC with clinical aggressiveness. CONCLUSION: We found that the prevalence of ret/PTC rearrangement (3/14, 21.4%) in papillary thyroid carcinomas from Korea was similar to those recently reported in other nations. ret/PTC rearrangement may not affect biological behaviors of papillary thyroid carcinomas.

- A Case of Acromegaly with Graves' Disease.
- Jae Hoon Chung, Kwang Won Kim, Byoung Joon Kim, Sung Hoon Kim, Myung Sik Lee, Moon Gyu Lee, Yong Ki Min, Jong Hyun Kim, Eun Young Oh, Yun Jae Chung, Sang Soo Bae
- J Korean Endocr Soc. 1998;13(3):432-438. Published online January 1, 2001
- 1,319 View
- 25 Download
-
 Abstract
Abstract
 PDF
PDF - Goiter is present in 25-50% of patients with acromegaly, which probably results from IGF- I stimulation of thyroid cell growth. These goiters are usually non-toxic but there have been well documented cases of co-existent hyperthyroidism and acromegaly. Graves disease with acromegaly has been rarely reported compared with the other type of hyperthyroidism due to increased tumoral secretion of TSH. We experienced a 44-year-old woman who presented with Graves disease and acromegaly. Basal serum GH and IGF-I concentrations were 10.8 pg/L and 571.82 ng/mL, respectively (reference value: (5 mg/L and 130-354 ng/mL, respectively). GH was not suppressed less than 2 pg/L during oral glucose loading test. GH was stimulated by TRH. Postcontrast sellar MRI demonstrated ovoid-shaped low signal intensity nodule measuring O.8 cm in diameter in left side of pituitary gland. Thyroid scan(131I) showed enlarged thyroid with increased radioiodine uptake (61.3%). Histologic examination showed acidophilic adenoma. GH and prolactin were positive on immunohistochemical staining. GH was suppressed less than 2.26 mg/L by oral glucose loading following operation. The patient has been followed with antithyroid drug(PTU) medication after operation(TSA).

- A Case of Acromegaly Caused by Mixed Gangliocytoma-Adenoma of the Pituitary Gland.
- Jae Hoon Chung, Kwang Won Kim, Byoung Joon Kim, Sung Hoon Kim, Myung Sik Lee, Moon Gyu Lee, Yong Ki Min, Yeon Rim Seo, Jong Hyun Kim, Sang Jong Park
- J Korean Endocr Soc. 1998;13(3):423-431. Published online January 1, 2001
- 980 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - The tumors containing ganglion cells are rare in the pituitary gland. These tumors are divided into two groups. The first group is the cases of mixed gangliocytoma-adenoma that contained both gangliocytoma and pituitary adenoma elements in the same tumor and the second group is those of gangliocytoma that contained only gangliocytoma element. Since the first description by Kiyono in 1926, 45 cases have been reported. The most common presentation of these tumors is acromegaly and the cases of Cushings disease and galactorrhea-amenorrhea also have been reported. In immunohistochemical study, hypothalamic-releasing hormones are stained in gangliocytoma cells and adenohypophyseal hormones are stained in adenoma cells. The releasing hormones stained in gangliocytoma element and the pituitary hormones stained in adenoma elements are usually closely related but unrelated cases also have been reported. We report a case of a 41 year-old lady with acromegaly which was diagnosed as mixed gangliocytoma-adenoma after surgical removal of the pituitary tumor.

- A Frequency of Hypothyroidism in a Population of Hypercholesterolemin Subjects.
- Jae Hoon Chung, Kwang Won Kim, Byoung Joon Kim, Sung Hoon Kim, Kyung Ah Kim, Myung Sik Lee, Moon Gyu Lee, Yong Ki Min, Yun Ho Choi, Myung Hee Shin
- J Korean Endocr Soc. 1998;13(3):351-358. Published online January 1, 2001
- 1,052 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Hypothyroidism is a treatable cause of secondary hyperlipidemia. The lipid profile usually seen is an increased total and low density lipoprotein(LDL) cholesterol, and the plasma triglyceride may also be increased. Hypercholesterolemia associated with hypothyroidism is an important factor in the pathogenesis of coronary artery disease(CAD). And the hyperchole-sterolemia caused by hypothyroidism is potentially reversible by thyroid hormone replacement therapy. Hypothyroidism should be ruled out by routine laboratory screening as a treatable cause of secondary hyperlipidemia and increased CAD risk. We carried out this study aimed at evaluating the frequency of hypothyroidism and its relationship with serum cholesterol concentration in Koreans. METHODS: We investigated 15028(men 8273, women 6755) Korean subjects who visited our hospital center for health promotion during an one year period(from January 1, 1996, to December 31, 1996). Among them, we analyzed 6756 hypercholesterolemic subjects whose serum cholesterol levels were greater than 200 mg/dL. They performed thyroid function tests(total T, T4, and TSH) and lipid profiles(total cholesterol, triglyceride and HDL-cholesterol) were measured by enzyme assay. We defined hypothyroidism by serum thyrotropin values greater than 5 U/mL. RESULTS: The observed prevalence of hypothyroidism was 2.4%(163/6756). Among those with high TSH levels, 17(10.4%) had overt hypothyroidism with a low T4 (below 6 g/dL) level. As we analyzed the frequency of hypothyroidism according to cholesterol range by 20 mg/dL, the frequency was significantly increased in the group whose serum cholesterol levels were greater than 300 mg/dL, especially in women over 50 years of age. Analysis of lipid parameters showed that hypertriglyceridemia was frequent and hyperHDLaemia was observed in hypothyroidic populations. CONCLUSION: Screening for hypothyroidism by measurement of thyrotropin values is of particular importance in patients with hypercholesterolemia. And the frequency of hypothyroidism was more significantly increased in whose serum cholesterol levels were greater than 300 mg/dL, especially in the group of women over 50 years of age.


 KES
KES

 First
First Prev
Prev



